Imagine your heart can no longer pump enough blood to your vital organs. Even minimal exercise tires you out, and you’re often short of breath when lying flat. Your lungs are accumulating fluid. Your kidneys and liver are impaired.
You’ve been hospitalized and started on an intravenous drug that improves your heart’s ability to contract. It has helped, but it is not a long-term solution. You need a new heart.
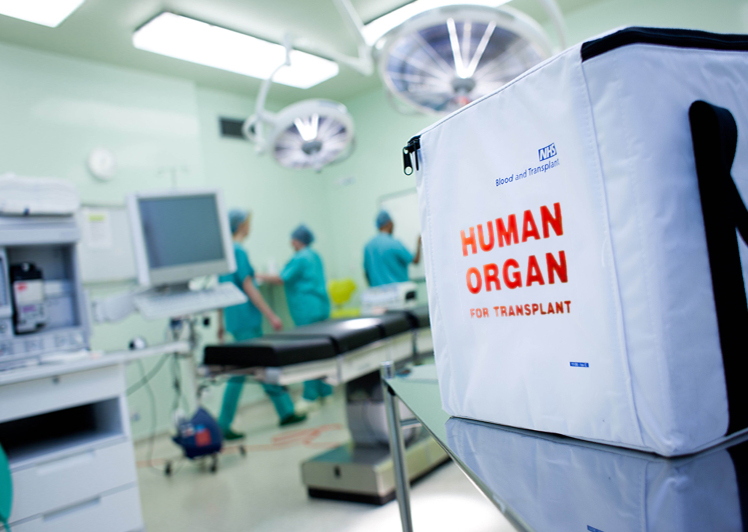
You’re a good candidate, but there is a problem: a chronic shortage of donor hearts. In 2014, for example, about 6,950 Americans were approved for heart transplants, but only about 2,250 donor hearts became available. You need to move higher up on the list.
I’m your doctor. I want to help you get you a heart. But I face an ethical dilemma: Do I ramp up your medical treatment, even beyond what I consider necessary, to bump you higher on the list?
Aiming for Status 1A
The United Network for Organ Sharing, or UNOS, has established criteria to make sure that donor hearts go to patients with the most severe disease. These criteria are based on which treatments a doctor has prescribed, on the assumption that they’re a good indication of how critical the illness is.
Generally, that’s a fair assumption. Except that the system itself creates a perverse incentive.
It works like this: Your place on the waiting list for hearts depends on your “status.” If you weren’t getting that IV drug, you’d be considered “Status 2,” and your median wait time for a heart would be 630 days. Not good.
You’re on the IV drug, though, so you’re considered “Status 1.” But “Status 1” is divided into two more categories: If you’re on a low dose of the IV drug, you’re classified as “1B,” cutting your median wait to 301 days. That’s where you are now. Better, but still not great.
But if you were in an intensive care unit, receiving a high dose of your IV drug, and you had a catheter placed in your pulmonary artery to monitor cardiac performance, you would be “Status 1A.” Your median wait would drop to 110 days.
So you’re unlikely to get a heart anytime soon unless you can be listed as 1A. And in your case, if you weren’t up for a transplant, there would be no call to implant a pulmonary-artery catheter; it’s uncomfortable (it is inserted through your neck or under your collarbone) and carries a risk of infection. There would also be no call to raise your dose of the IV drug that’s helping your heart contract; when used long term, higher doses can increase the risk of sudden cardiac death.
But I have to balance these risks against the danger of your having to wait three times as long for a transplant if you remain 1B. That means spending an additional 291 days on the waiting list, during which your condition may deteriorate. You may end up needing a mechanical pump or an artificial heart, both of which would entail major cardiac surgery and potentially serious complications. And you may die.
When I take all that into account, the risks of keeping you waiting at 1B seem higher than the risks of placing a pulmonary-artery catheter and raising the dose of your IV medication to make you 1A.
This is the system I have to navigate.
So, as your doctor, even though these measures aren’t medically indicated, do I admit you to intensive care, insert a pulmonary-artery catheter and increase your medication to qualify you for 1A status? And if I do, is it ethical?
Read Full Article – Source: Doctors Game The System To Help Their Own Transplant Patients : Shots – Health News : NPR
By – MATTHEW MOVSESIAN
Photo Credit – NHSBT